A day in the life of an Occupational Therapist on Critical Care
Rosie Thurlow, Occupational Therapist at DCH, and Lucy Smith, Occupational Therapist at UHS, tell us more about their role in Critical Care.
Occupational Therapists (OT) are interested in how people occupy their time. People occupy their time with Activities of Daily Living (ADLs). Think about how many activities you’ve engaged in since you woke up today? Even in the first 10 minutes of waking we complete multiple ADLs: Brushing teeth, showering, snoozing the alarm clock! Think about all the physical and cognitive abilities those tasks require.
Now think about patients of Critical Care. They are deprived of so much engagement in ADLs. They might struggle to engage with ADLs due to cognitive or physical impairments and due to the critical care environment. Those we encourage them to engage in are generally painful, frightening or confusing.
Occupational therapists are trained in physical and cognitive assessment and rehabilitation. The critical care patient group can have ongoing multi-factorial issues from their critical illness and OTs are well equipped to support with these.
Occupational therapy provision in critical care still varies nationally, despite guidelines suggesting OTs should be involved at every step of a patient’s journey from Critical Care. At University Hospital of Southampton (UHS) we have 0.6 band 7 and 1.0 rotational band 6 OT covering 32 beds on the General Intensive Care Unit (GICU). At Dorchester County Hospital we have 2 x 0.6 band 7 OTs covering 12 beds (but we also cover all of the medical wards).

Typical interventions for OT on Critical Care include:
Holistic assessment of how critical illness is impacting an individual and how this affects their ability to participate in ADLs (including a detailed social history and occupational profile)
Using function within rehabilitation which may have a physical or cognitive focus.
Cognitive assessments and rehabilitation.
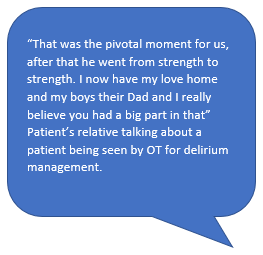
Nonpharmacological management of delirium including orientation boards, structure and routine, timetables, engagement in normal activities of daily living, educating and involving family.
Upper limb rehabilitation targeting range of movement, power, tone or oedema management.
Tone management including splinting.
Specialist seating assessments.
Humanising bed spaces including using photos, this is me booklets, meaningful music or familiar smells.
Wellbeing support including coping strategies for anxiety or low mood, sleep hygiene, facilitating time off the unit.
Communication support including provision or education of alternative communication methods, joint sessions with Speech and Language Therapists (SALT) for cognitive communication assessments.
Discharge planning for those going home straight from critical care including end of life patients.